The magnitude of pandemic trauma to our healthcare workers ensures a long tail of depression, PTSD, drug addiction and suicide extending well into 2022.
The magnitude of pandemic trauma to our healthcare workers ensures a long tail of depression, PTSD, drug addiction and suicide extending well into 2022.
Now is the time to build the systems to cope with this delayed impact wave of COVID-19. We are not out of the woods when we reach herd immunity. It is only after the coast is clear that the psychiatric complications manifest in our physicians and staff.
In this short video, I will show you
- The Six Phases of the Human Emotional Response to Trauma
These delayed mental health complications happen in the wake of all disasters. - The Safety Net System all healthcare organizations must put in place NOW to be ready for the inevitable surge in mental health issues that will begin only after the virus is gone.
- How to tell if your Safety Net is working in just 15 seconds.
============
Are You Prepared for the Great Practice RESET of 2022?
Get the Tools and Support to Take Back Your Practice
in the Wake of the Pandemic
============
Physician Burnout, Suicide and the Post-Covid Trauma Wave
Help Us Spread the Word
SHARE this post on LinkedIn or this one on Facebook , or RT this Tweet on Twitter. THANK YOU!
VIDEO TRANSCRIPT:
Hello, this is Dr. Dike Drummond, at the home of the happy MD in beautiful Seattle, Washington, with a quick video on the connections between burnout, trauma, the COVID-19 pandemic, and two systems every healthcare delivery organization in the world needs to be putting in place right now. Because we actually know what's coming down the road.
A healthcare workplace is a unique work environment.
Everybody there has stood at one point in time at what I call the light workers fork in the road. Each of us stood at a place where we had a choice to make. You could go into health care, or you could do pretty much anything else. And all of us chose to go into healthcare to be a helper, a healer, a light worker.
We chose to ally our professional life in service to the forces of light in the universe, as they battle the forces of darkness: illness, suffering, death, dying, and family members crazed attempts to deal with those things. And because we're also there at the most traumatic and difficult point in other people's lives, it's also very common to become traumatized in either the training process or the practice of your craft, wherever you sit on the care team.
That's normal. Burnout and trauma are normal complications of being a light worker in the first place. And before the pandemic even started physician burnout rates were 40 to 50% in American physicians, and just as high and other members of the care team, nurses, nurse practitioners, PA’s. Everybody's stressed by the work that we do.
And then along comes the COVID-19 pandemic, a once in a century true disaster where big pieces of the healthcare delivery system were overwhelmed and swamped, sometimes repeatedly. Multiple deaths a day, multiple people being traumatized, the workers, the families, even the ancillary staff.
What I want you to know is we understand, although you may not have seen this before, we understand the human emotional response to disaster better than you might think.
I don't know if you remember, but think back to when you learned about Kubler Ross's stages of adjusting to the death and dying process. Where you first heard of the stages of Kubler Ross. It sort of gave you a structure to understand. You said “Yeah, that makes sense”. Well, there's actually six phases of the human emotional response to disaster. We know this from the disaster research from government agencies responding to disasters like tornadoes, and hurricanes and such. Let me share this with you all six phases, I think you'll be able to find yourself on this graph.
And let me tell you two, there's two support systems all healthcare organizations need to be putting in place right now, because we know what's coming in stage six, ready, here's the graph.
So here you go. It's called the Zunin and Myers after the researchers who developed it. Zunin and Myers six phases of the human emotional response to disaster.
And if you look, it's got a vertical axis, it's got a horizontal axis. Vertical is your emotional state, higher is positive, lower is more negative. And the horizontal axis is time. This goes from before the disaster hits, especially if you have a pre warning all the way to complete recovery of your emotional state after the disaster.
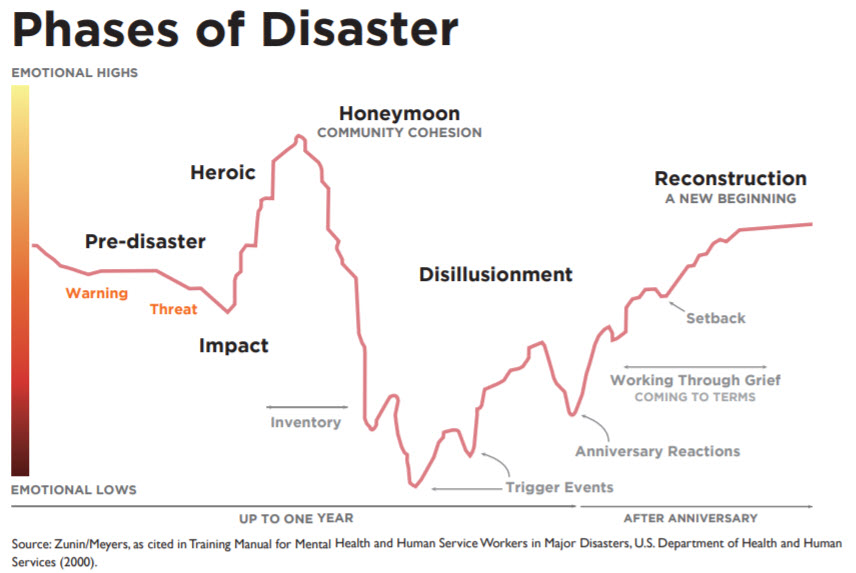
Let's just go through each of the phases one at a time, and describe what's going on and show you where they are in the graph.
The first phase is called pre disaster.
That's where you know something's coming in, you're bracing for impact you're preparing, laying in supplies. And in some cases, you actually end up in a hurry up and wait mode.
Phase number two is the impact phase.
That's where Wham the disaster hits. And it is met with shock and panic and disbelief and attempts at self-preservation. We circle the wagons and attempt to write out the impact.
Phase number three is called the hero phase
Where our adrenaline rises, and we gain together strength and clarity and cooperation all hands on deck in the emergency response. And, and if there was a dramatic impact at the start of the disaster, this is where you reconnect with your fellow survivors and friends and family. You can see who's survived with you.
Phase four is the honeymoon phase.
That's where you first begin to wrap your brain around the scope of the disaster. Survivors and the emergency responders bond with each other, but the impact is starting to creep in around the edges even despite the cooperation and camaraderie of Emergency Response.
Phase number five is the disillusionment phase.
This is where the true impact of the disaster and the things and people that you lost begin to sink in, you realize you are never going to be made whole again, you realize who has been lost and the economic wreckage. And if there was inadequate emergency response to this disaster, this can produce extreme outrage and set the stage for lasting resentment.
Phase six is reconstruction and recovery.
This is the last and longest stage. You realize you have to pull yourself up by your own bootstraps because the emergency response if it was a national emergency response has left town. Grief sets in. Recognition of both loss and your strengths that allowed you to survive the disaster become apparent.
Some of us will rise to the occasion at this point, but some of us will not. Because if to cope with the disaster, you picked up drugs and alcohol or slid into depression. Maybe even in the acute phase, there was suicides, you will struggle in the reconstruction phase when retraumatization and anniversary events begin to come through over time.
One of the fundamental features of the reconstruction and recovery phase is its time delay.
You can see in this graph, it's about 18 months to run from an acute disaster all the way through to the end of the recovery phase. And most of the depression and suicide and psychiatric morbidity of a disaster like this is on the upslope of the recovery phase a year or so delayed from the actual disaster itself.
And the thing that distinguishes COVID from singular disasters like a hurricane, a tornado, an earthquake, a terrorist attack, is it those are point disasters, where it hits fast and we recover from that point forward. COVID has rolled in in waves that last weeks at a time. And it exhausts and traumatizes the healthcare workers that are in the frontlines in ways that no tornado or hurricane could possibly hope to accomplish.
So, I've always advocated that all healthcare delivery organizations have in addition to their employee assistance plan their EAP, they need to have a crisis management plan for the physicians and the other providers who don't tend to use EAP. You should have that in place right now.
But as I talked to doctors and physician leaders around the country, I know that most healthcare delivery organizations do not have a crisis hotline. Even if they have a crisis hotline, if I ask somebody, what's the number nobody can ever tell me.
So here's what we have to do now use the crisis of this COVID pandemic, to begin to build out the crisis management system that we're going to need a year from now.
What we need now is to build out a 24/7 manned hotline with a triage professional there so that when people call in, they can have a survey administered and be triaged to the appropriate resources.
And we have to have a complete awareness plan of how to refer into the program.
And it would love it to be completely practical. So for instance, whatever your hotline is, print that number on a whole bunch of business cards, give a business card to everybody in the organization and a handful to every leader. So we're always carrying them and can hand them out if we're talking to somebody who's in distress.
So if I ask anybody in the front line, what's your hotline number, they can just reach in their pocket. And there it is.
And because it's much less likely for the healthcare worker to recognize their own burnout their own trauma, because the patient comes first and never show weakness, it's also important to get this hotline number in the hands of their families. And the best way I know of to do that is with a little refrigerator magnet, it's the same size as the business card, but you send it to the home address to the significant other spouse partner of the healthcare worker so that they have it on their refrigerator at home. Because your spouse, your partner is more likely to call to get you help than you are to call for yourself.
Everybody has to be taught how to refer into the program.
And behind the crisis hotline, there should be a whole network of healthcare professionals to take care of the people that come through the hotline number.
Now this this is typically covered for rank-and-file employees in the employee assistance program. EAP. But I'll tell you doctors don't use that. So we need to create a parallel system for the physicians.
And then another thing that has to happen is this we have to begin to normalize the conversation around Stress, Stress Management, burnout, getting help depression, suicidal ideation, we have to let people know that in times like these, you must take care of yourself first. It's no good having you depressed and suicidal and struggling to continue to show up and take care of patients, because you simply can't give what you ain't got. And when the masks come down in the airplane, who puts their mask on first? Yes, it's you.
We have to teach people that asking for help is not a sign of weakness. Asking for help is what we expect. And we're here to have your back and take care of you if you need help right now.
So please, use this current crisis to build out a crisis intervention program. So that 12 to 18 months from now we're prepared and everybody knows the number and how to refer into it.
Now, how do we know this is going to happen?
Well, if you look at the SARS epidemic in Toronto in 2003 2004, compared to the to the COVID crisis here, we're we're at this point in time as I'm filming this, that 300,000 deaths, the SARS epidemic in Toronto was only 450 people who died. But they tracked the staff of the hospitals in the wake of that disaster and saw this delayed depression, suicide and other psychiatric morbidities a year later.
So please, if you don't have a crisis intervention program with a 24 hour hotline, or if you have one and you don't know the number, please commit to taking an action step in the wake of this video.
- Who do you need to show this video to on your leadership team to get this process started?
- Who do you need to reach out to on your work team who's obviously struggling to show them that you have their back and ask if you can help support them?
- How can we come together as work teams, as light workers to take care of each other in this crisis?
- And how can we build a system to do that down the road when things are going to be even more desperate.
So that's it for now, please do something to raise awareness in your organization. Now that you've seen this video, and my fingers are crossed. I'm praying that the pandemic we're in the midst of right now does slack and by the end of 2020 into 2021, so that we can get some breathing space, get the vaccines on board, reach herd immunity, and get out of this long dark tunnel.
That's it for now. Till I see you in another training video. Keep breathing. Stay safe and have a great rest of your day.
============
PLEASE LEAVE A COMMENT
- Does your organization have a crisis hotline for physicians?
- Do you have a business card or fridge magnet with the hotline number?
- Who would you talk to in order to make that happen?